
Therapeutic Method And Outcomes
Therapeutic method and outcomes of using an access port device in laparoscopic surgery for small bowel obstruction
Ryosuke Nakata1, 2*, Masaki Koizumi1, Hideyuki Hagiwara1, Naoto Chihara2, Yuji Kurihara2,3, Hideyuki Suzuki2, Nobuhiko Taniai2
1Department of surgery, Ebina general hospital, Ebina-shi, Kanagawa, Japan
2Institute of Gastroenterology, Nippon Medical School Musashikosugi Hospita, Kawasaki, Kanagawa, Japan
3Department of Surgery, Yotsukaido Tokushukai Hospital, Chiba, Japan
Abstract. The use of laparoscopic surgery has spread at an accelerating rate due to its minimally invasive nature and the early rehabilitation that it affords. Whether laparoscopic surgery is feasible for small bowel obstruction (SBO), however, remains controversial. This retrospective study presents our experiences in the laparoscopic treatment of SBO to assess the feasibility, efficacy, and clinical outcomes in comparison with open surgery and to present the author’s surgical methods regarding the use of an access port device. From April 2014 to March 2015, 36 patients who were admitted to our department for SBO underwent surgical treatment. The operating surgeon attempted to detect a transitional point between the distended and collapsed bowel with preoperative computed tomography and then decided whether to perform laparoscopic surgery (LS; n=19) or open surgery (OS; n=17). Our laparoscopic surgical technique for SBO used an access port device and a small umbilical incision of 1.5 – 2.5 cm. The background information of the patients and the postoperative outcomes were collected and subjected to a statistical analysis. Postoperative adhesions were the cause of the obstruction in 23 patients. Incarcerated inguinal and internal hernias were identified in 6 and 4 cases, respectively, and a tumor, intussusception and volvulus of the small intestine were identified in one case each. Three patients (15.8%) of the LS group were converted to laparotomy due to dense adhesion in one case and adhesion below the umbilicus in two cases. Six patients required segmental resection through the access device at the umbilicus. No statistically significant differences were found between LS and OS in the operative time (LS vs. OS; 85.3 min vs. 88.2 min, p=0.8570), postoperative complication rate (5.26% vs. 5.88%, p=0.9355), or the postoperative hospital stay (10.3 days vs. 15.9 days, p= 0.3524). There was a significant difference in the mean timing of oral re-intake after surgery and the amount of intraoperative blood loss (2.5 days vs. 4.5 days p<0.05, 3.8 g vs. 92.9 g p<0.05, respectively). In conclusion, our results indicate that LS with an access port device was suitable for the treatment of SBO in most patients, and that it is useful both as a diagnostic tool and as a therapeutic surgical approach.
Keywords: Small bowel obstruction, laparoscopy, acute abdomen
Introduction
Small bowel obstruction (SBO) is a relatively common disease in several conditions of acute abdomen and it results in emergency admission [1-4]. The clinical course is somewhat unfavorable, with a morbidity rate of about 30% if strangulation is present [5]. The most common causes of SBO are postoperative adhesions, which are present in 83.2% of all patients. This is not surprising given the marked increase in the number of elective surgeries for elective hernia repair to prevent incarcerated intestinal obstruction [6]. Other causes of SBO include abdominal wall hernia and malignant tumors which account for 3.1% and 2.9% of patients, respectively [7-9].
Open adhesiolysis is the conventional surgical approach for SBO patients who do not respond well to conservative therapy and in whom there are clinical findings of incarceration or perforation of intestine [10-12]. However, a potential problem when operating on patients with adhesion is that the new operation may cause even more adhesion. Several clinical studies and most experimental studies have shown that adhesive formation is reduced in laparoscopic surgery (LS) in comparison to open surgery (OS) [13]. On the other hand, surgeons consider the performance of adhesiolysis in LS to be unfavorable due to the risk of iatrogenic bowel injury, the difficulty of maintaining view field
and their restricted ability to manipulate the instruments [7].
In 1991, Bastug et al. [14] presented the first report on laparoscopic surgery for SBO. From that time, numerous reports have shown the feasibility and utility of the laparoscopic approach for the management of SBO [13, 15-17]. In addition, with increased experience and technical advances in laparoscopic techniques and instrumentation, morbid obesity and previous abdominal surgery are no longer considered to be contraindications for laparoscopy [15].
We herein present our experiences with LS for SBO of various etiologies to assess the feasibility, efficacy, and clinical outcomes associated with this therapeutic method and present our methodology.
Materials and Methods
We respectively reviewed the clinical records of 36 patients who were hospitalized in our department from April 2014 to March 2015 for SBO and who underwent surgical treatment due to clinical findings of intestinal ischemia or the failure of conservative management.
The diagnosis of SBO was performed based on the
patient’s complete medical history and a physical examination combined with laboratory blood tests and imaging studies. Abdominal computed tomography (CT)
was a particularly useful modality for diagnosing and detecting the location of obstructions. Patient management included nasogastric intubation, the placement of a long intestine suction tube, and vigorous resuscitation with the administration of intravenous fluid and electrolytes. Patients with virgin abdomens usually underwent immediate laparoscopic exploration. In addition, the presence of signs of peritoneal irritation or an elevated and rising white blood cell count prompted urgent surgery. When elective surgery was indicated, conservative measures were continued 5-7 days. If the obstruction did not resolve with this period, surgical intervention was performed. The surgical method (LS or OS) was chosen by the operating surgeon based on the clinical findings of massive abdominal distension or if there was a risk of dense broad adhesion. The administration of antibiotics was initiated in accordance with the indications of each patient.
The preoperative patient demographic characteristics, including sex, age, body mass index, preoperative intubation with a long intestinal tube, and previous abdominal surgery were included in the analysis. The patients were evaluated for perioperative risks based on the statuses of the American society of Anesthesiologists (ASA). Clinical preoperative data, including the white blood cell count (WBC), and the C-reactive protein (CRP), creatine phosphorus kinase (CPK), lactate dehydrogenase (LDH), and total bilirubin (T-bil) levels were also retrospectively compared between the LS group and the OS group.
The operative data, including the operative time, amount of blood loss, the performance of bowel resection, the timing of the restarting of oral-intake and postoperative hospital stay were compared between the LS group, OS group and the conversion laparotomy group. Surgical procedures All operations were performed by experienced laparoscopic surgeons or by residents under supervision. Detailed informed consent for laparoscopy and possible conversion was obtained from all patients. Patient positioning for laparoscopic surgery for adhesiolysis is similar to that of other laparoscopic procedures such as appendectomy. All patients underwent general anesthesia and were placed in the supine position with one or both arms alongside of the patient’s body. The placement of the operator and monitor was determined by the findings of the

obstructive location in preoperative abdominal CT. The surgical operator stood opposite to the monitor, which was placed on the same side as the obstruction. The camera operator stood next to the surgeon.
A skin incision of 2-3 cm was made in the umbilical region. We used an EZ-access with a Lap-protector (Hakko Medical Inc., Chikuma, Japan) as the umbilical access device. Two 5 mm trocars were placed through the EZ-access device for a 5 mm laparoscope and a 5 mm instrument. After attaching the EZ access device to the Lap-protector, pneumoperitoneum was established and maintained at 10 mmHg using CO2. A 5 mm trocar was placed under laparoscopic guidance into the lower abdomen (Figure 1). Two types of laparoscope, a flexible or a 30º side-view 5-mm telescope, were used. The other essential instruments included atraumatic graspers, scissors with cautery capability, and an ultrasonic dissector.
After sufficient instruments were prepared in the abdomen, the procedure began with detecting and approaching the point of obstruction. The surgeon should be mindful that the dilated and edematous bowel is easily injured by small instruments. To the extent that was possible, the small bowel was run with atraumatic graspers in a retrograde manner from the cecum to detect the point of obstruction. In addition, the grasping of the mesentery to manipulate the bowel also decreases the incidence of bowel perforation.
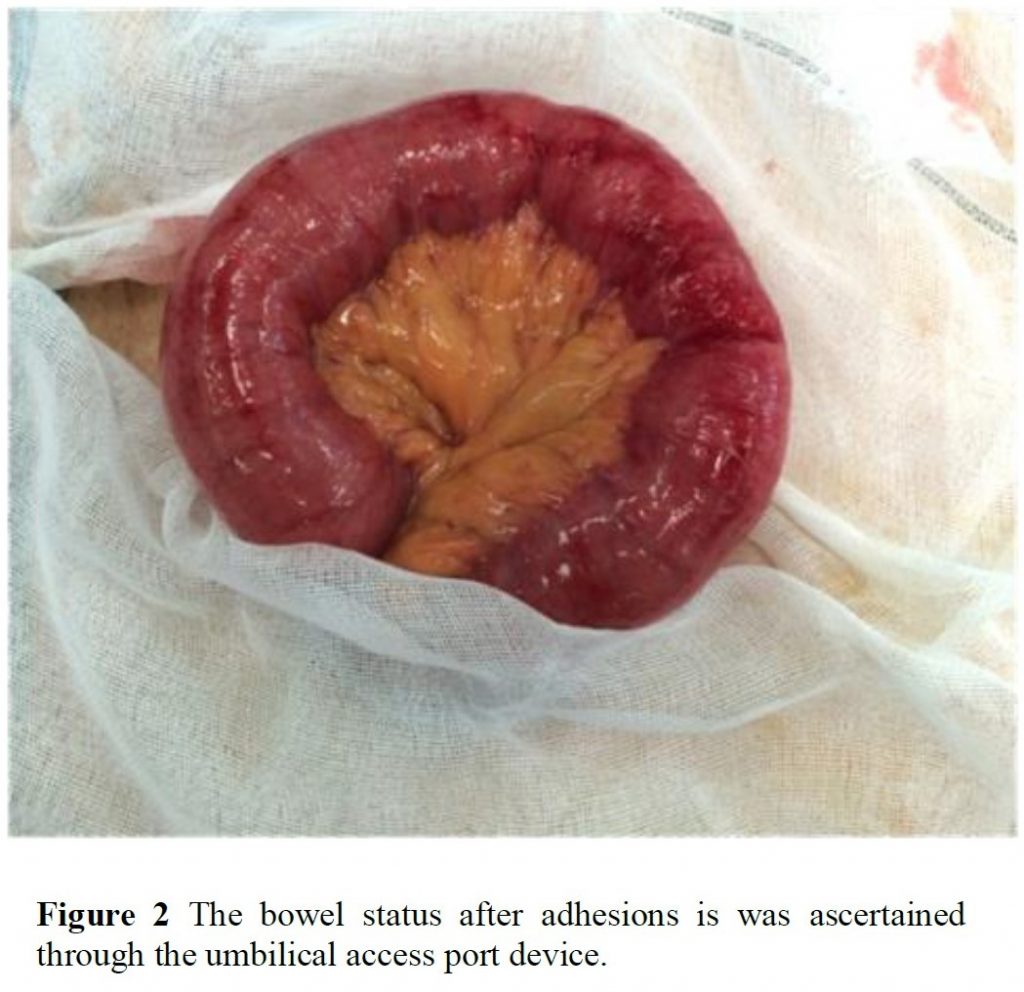
For cases of simple adhesive intestinal obstruction, a combination of a sharp dissection with the sensible use of electrocautery or an ultrasonic scalpel was applied to treat adhesiolysis. In such cases, it is necessary to consider that electrical intestinal injury may not be recognized immediately and may present as a delayed perforation. After adhesiolysis, the state of the lysed intestinal serosa can be assessed through the umbilical Lap-protector. The indications for repair and resection are evaluated based on the direct visual findings and palpation.
For cases of abdominal wall hernia, obstruction is improved by the laparoscopic reduction of the incarcerated hernia. In cases where reduction was possible, we
performed a laparoscopic evaluation of the viability of the incarcerated bowel segment based on the color, the presence of peristalsis, and venous congestion. In cases where bowel resection was not required, TAPP was performed in the usual manner. On the other hand, when obviously necrotic intestine was detected, immediate bowel resection and anastomosis was performed extracorporeally through an umbilical Lap-protector. The same treatment was used when any tumors were identified as the cause of obstruction.
The nasogastric tube was left in place, and the patient was maintained on intravenous fluids, with nothing by mouth until the return of bowel function was heralded by bowel sounds or the passage of flatus. Subsequently, the nasogastric tube was removed, and the diet was advanced as tolerated.
Statistical analysis
Statistical analyses were performed to compare the characteristics and results of the LS and OS groups. All statistical analyses were performed using the JMP ® 11.0.0 software program (SAS Institute Japan, Tokyo, Japan). Patient characteristic and perioperative variables were compared in a univariate analysis to determine the association of each variable with the outcome. Fisher’s exact test and the Mann–Whitney U test were performed. A p value of <0.05 was considered to be statistically significant.
Results
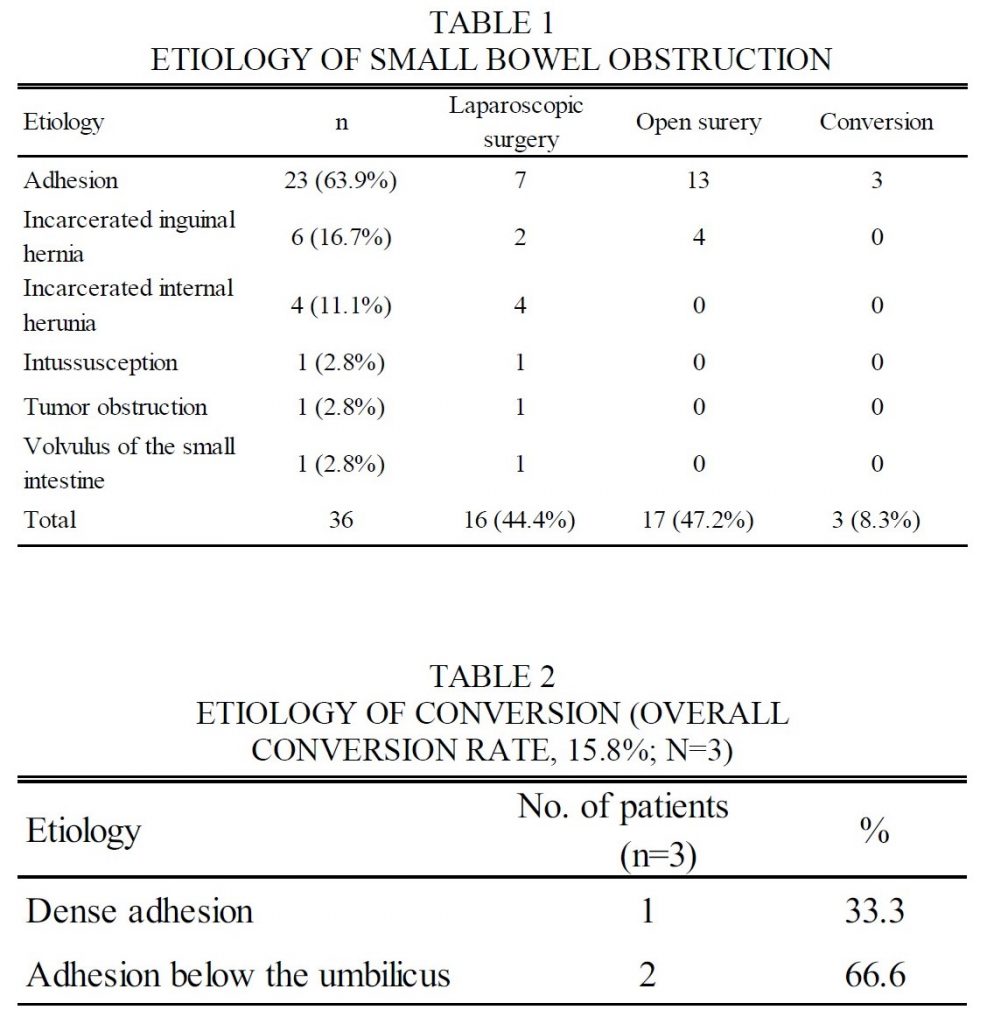
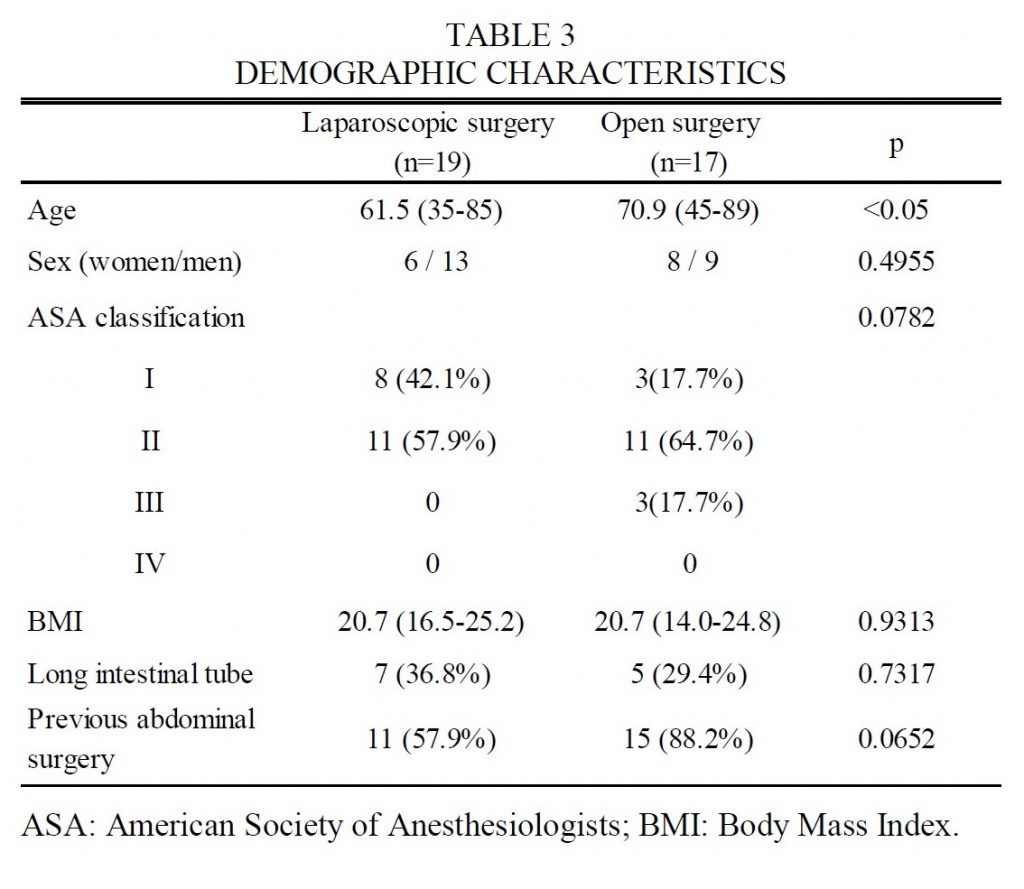
The etiologies of SBO are outlined in Table 1. Postoperative adhesion was identified in 63.9% of patients (n=23), as well as incarcerated inguinal hernia (n=6), incarcerated internal hernia (n=4), intussusception (n=1), tumor (n=1), and volvulus of the small intestine (n=1). Laparoscopy was initially attempted in 10 patients with adhesive ileus. The other 13 patients who had a medical history of repeated ileus underwent open surgery due to suspected dense adhesion. The conversion rate from laparoscopy to laparotomy was 15.8% (n=3). The reasons for conversion, which are shown in Table 2, were dense adhesion (n=1), and adhesion below the umbilicus (n=2). In the umbilical adhesion patients, exploratory laparoscopy with an access port device was performed to confirm that no other obstructions were present after adhesiolysis.
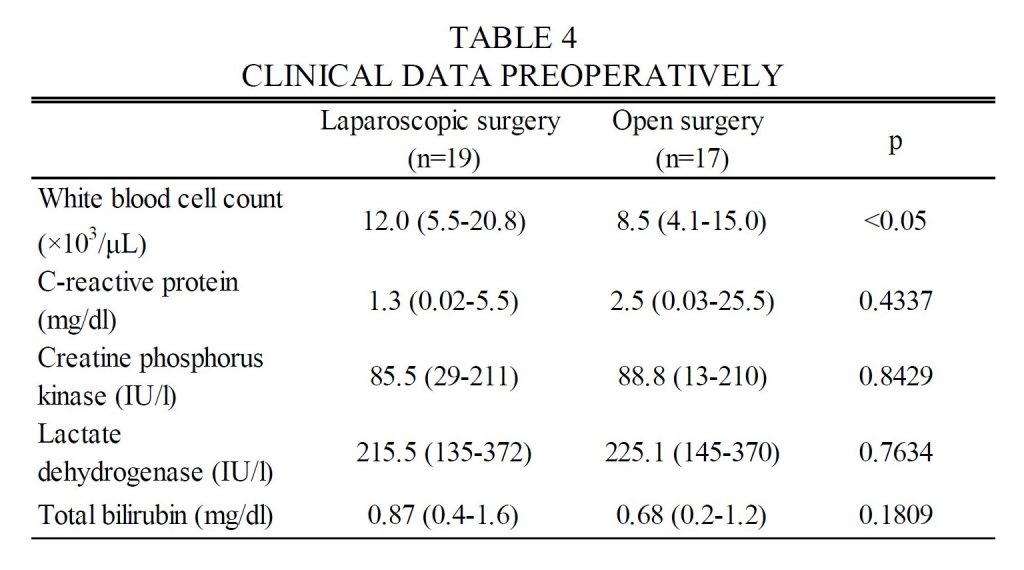
The patient characteristics and preoperative clinical data are listed in Tables 3 and 4. The patients in the LS group were younger than the patients in the OS group. There was no significant differences in the other characteristics of the patients in the two groups. Regarding the laboratory findings, the white blood cell count was higher in the LS group than OS group.
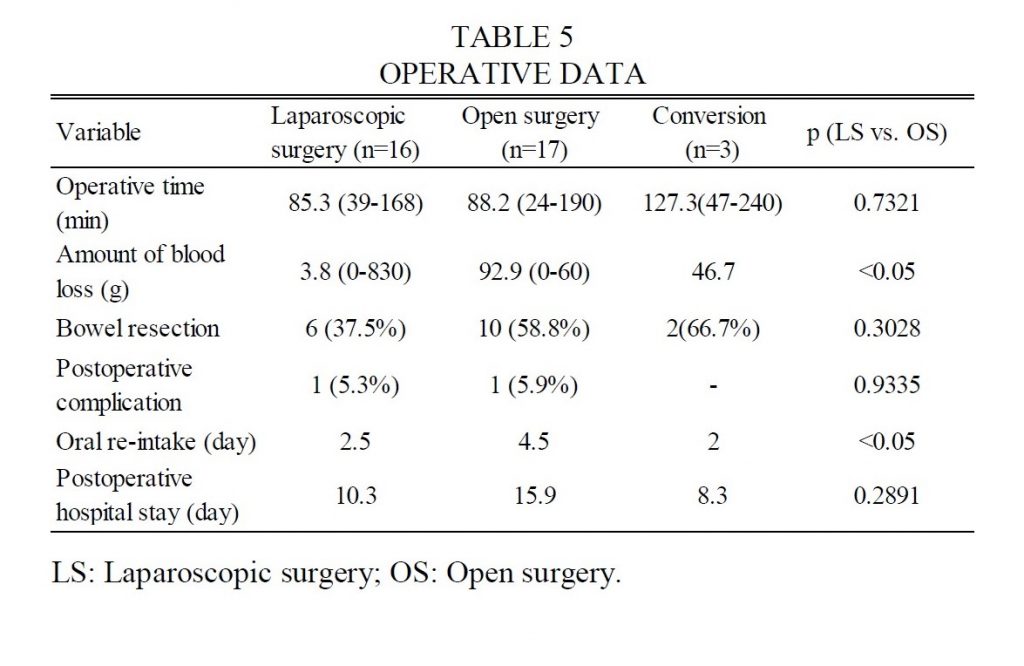
The perioperative data are shown in Table 5. The amount of intraoperative blood loss was significantly lower in the LS group than in the OS group (3.8 g vs. 92.9 g, p=0.0017). Oral re-intake occurred more quickly in the LS group than in the OS group (2.5 days vs. 4.5 days, p<0.05). Each of the two groups had one case of postoperative complication that was not lethal but which delayed re-oral intake. There were no significant differences between the

The patient characteristics and preoperative clinical data are listed in Tables 3 and 4. The patients in the LS group were younger than the patients in the OS group. There was no significant differences in the other characteristics of the patients in the two groups. Regarding the laboratory findings, the white blood cell count was higher in the LS group than OS group.
The perioperative data are shown in Table 5. The amount of intraoperative blood loss was significantly lower in the LS group than in the OS group (3.8 g vs. 92.9 g, p=0.0017). Oral re-intake occurred more quickly in the LS group than in the OS group (2.5 days vs. 4.5 days, p<0.05). Each of the two groups had one case of postoperative complication that was not lethal but which delayed re-oral intake. There were no significant differences between the two groups with regard to the mean operative time, the number of cases in which bowel resection was performed or the duration of postoperative hospital stay (10.3 days vs. 15.9 days, p= 0.3524).
Discussion
In this retrospective study, we evaluated the feasibility, efficacy and clinical outcome of the laparoscopic surgery for SBO in comparison to open surgery and presented our methodology. The main cause of SBO was adhesion (63.9% of patients). In the LS group, the overall conversion rate was 15.8%. The rate of postoperative complications did not differ significantly between the LS and OS groups (5.3% vs. 5.9% p=0.9335). All of the patients survived the surgery. There was a significant difference in the timing of postoperative oral re-intake; the LS group achieved oral re-intake more quickly than the OS group (2.5 days vs. 4.5 days, p=0.0374). This indicates that bowel function recovered faster in the LS group, which is in line with a previous report [18]. However, we did not find any significant difference in the postoperative hospital stay. The earlier oral re-intake of the LS group suggests the possibility that the hospital stay may be shortened.
Laparotomy has traditionally been the standard surgical intervention for SBO when conservative therapies fail. On the other hand, the laparoscopic approach for SBO is associated with a potential problem in that it may cause further adhesion. A large number of clinical and experimental studies have shown a reduction in adhesion formation after laparoscopic surgery in comparison to open surgery [13]. In addition, laparoscopic surgery for bowel operations has been shown to significantly reduce the incidence of SBO in comparison to open surgery [16]. These data show that LS is an attractive and reasonable therapeutic option for SBO.
Beck et al. reported in a postoperative trial that in 63% of laparotomy incisions, the length of the incision was involved in the formation of adhesion in the intraperitoneal region [19]. Furthermore, the incidence of ventral hernia after laparotomy is reported to be from 11% to 20%, whereas that in laparoscopic surgery is reported to be 2.5% [16,20,21]. The additional benefits of laparoscopic approach are reported to be a decreased incidence of wound infection and postoperative pneumonia, a more rapid return of bowel function, and a shorter hospital stay [18]. All suspected cases of intestinal obstruction can initially be approached by laparoscopy. In experienced hands, the laparoscopic management of SBO is successful; 66% of cases are performed without conversion [7].
As a controversial point, there are measures that may be implemented to prevent intestinal perforation at the time of the first trocar insertion [22-26]. We conducted the preoperative ultrasound mapping of the adhesions as a way of ascertaining the presence of dense adhesion at the umbilicus. In addition, in our methodology, the first trocar was set with EZ-access after the insertion of a Lap-protector into the umbilical incision. Because the first trocar was inserted under direct vision, none of the patients in our series suffered an intestinal injury.
Another safety-related issue concerning laparoscopic surgery in SBO patients with bowel distension is the instrumentation and handling of the bowel, due to the increased risk of perforation. Wullstein et al. reported a 26.9% rate of bowel injury in patients who underwent LS, in comparison to a 13.5% rate in patients who underwent laparotomy [27]. Although missed enterotomy can occur in association with laparotomy, the incidence is higher with laparoscopic surgery. However, the risk of bowel injury can be diminished with good surgical practices, which include avoiding the use of electrocautery, minimizing the grasping of the dilated bowel, manipulating the bowel using atraumatic graspers and by handling the mesentery whenever possible. This indicates that during laparoscopic surgery for SBO, the surgeon needs to be careful in the handling of bowel distension and in ascertaining the presence of bowel injury after adhesiolysis. We should pay attention to the possibility of thermal injury to the bowel due to the use of a monopolar electrocautery or a harmonic scalpel. In our methodology, it is easy to ascertain the presence of bowel injury through the umbilical access device. If the injury is detected or suspected, the bowel repair or resection can be performed concurrently. For the 8 patients of the LS group, some procedures were conducted through the umbilical access port device. Six patients required bowel resection and anastomosis for enterotomy with adhesiolysis, necrotic change for ischemia or an intestinal tumor. In two patients, the bowel status was ascertained with direct vision after the releasing strangulation. It was not hard to move the bowel through the small umbilical incision (approximately 2 cm) after the reduction.
In our study, three patients were converted to laparotomy before reduction. The reasons for conversion were dense adhesion in one patient, and adhesion below the umbilicus in two patients. In the umbilical adhesion patients, adhesiolysis was performed at the time of the insertion of the Lap-protector. Exploratory laparoscopy was performed with access port devices after adhesiolysis to confirm that there were no other obstructions. Exploratory laparoscopy can explore the intraperitoneal region more widely than open adhesiolysis or mini-laparotomy. It is considered that this procedure can lead to a reduction in the number of cases of reoperation for multiple obstructions. In a recently published review, Ghosheh et al. reported that 356 of 1,061 patients who underwent laparoscopy for acute SBO required conversion to open laparotomy (conversion rate, 33.5%) [7]. Conversion was most frequently due to dense adhesions (27.7%), followed by the need for bowel resection (23.1%) as a result of injury, ischemia, gangrene, and other causes.
In our procedure, another 5 mm skin incision was positioned on the lower abdomen to assist the surgeon. The skin incision became less noticeable after 2 weeks. Setting a 5 mm trocar upon the lower abdomen allowed the operator to maintain eye-hand and hand-hand coordination. In addition, the basic principle of triangulation of instrumentation is also maintained and it avoids instrument interference. When drain placement is required, it can be inserted into the skin incision on the lower abdomen.
A sufficient preoperative examination, such as abdominal CT or ultrasound mapping, is important in LS for SBO. Several studies have demonstrated the value of CT in confirming the diagnosis and revealing the cause of
SBO [28,29]. Moreover, Jerome et al. reported that MPR can increase both the accuracy and confidence in the location of the transition zone in CT of SBO; the authors reported that the accuracy of transition zone location was increased from 90% to 93% [30]. The preoperative detection of the transition zone is useful for detecting the origin of SBO with laparoscopy.
With an adequate preoperative examination, it is possible to provide sufficient therapy for each patient. The present study is associated with several limitations. Given that the assignment to the laparoscopic group was non-random, there is concern that overall healthier individuals were more likely to be selected for laparoscopic surgery than their sicker counterparts. We noted that patients undergoing laparoscopic adhesiolysis were more likely to be younger than the patients who underwent open surgery (61.5 vs. 70.9, p=0.0439). Despite these limitations, this retrospective study shows the feasibility of laparoscopic surgery for SBO and the efficacy of the use of an access port device at the umbilicus in selected adaptive patient, in whom preoperative examinations have been performed.
Conclusion
Laparoscopic adhesiolysis in SBO is a feasible treatment strategy, but is only convenient if it is performed in selected patients after a careful preoperative examination. Atraumatic manipulation and confirmation of intestinal injury were important in order to avoid postoperative complications. Our methodology of using an access port device overcomes these important challenges and is considered to be a suitable and reasonable method for performing laparoscopic adhesiolysis.
Conflict of Interest
The authors declare no conflicts of interest or financial ties in association with the present study.
References
1. Al-Mulhim AA. Laparoscopic management of acute small bowel obstruction. Surg Endosc 14:157-160, 2000.
2. Hawthorn IE. Abdominal pain as a cause of acute admis- sion to hospital. J R Coll Surg Edinb 37:389-393, 1992.
3. Mucha P Jr. Small intestinal obstruction. Surg Clin North Am 67:597-620, 1987.
4. Ellis H. The causes and prevention of intestinal adhesions. Br J Surg 69:241-243, 1982.
5. Bailey IS, Rhodes M, O’Rourke N, Nathanson L, Fielding G. Laparoscopic management of acute small bowel obstruction. Br J Surg 85:84-87, 1998.
6. Franklin ME Jr, Gonzalez JJ Jr, Miter DB, Glass JL, Paulson D. Laparoscopic diagnosis and treatment of intestinal obstruction. Surg Endosc 18:26-30, 2004.
7. Ghosheh B, Salameh J. Laparoscopic approach to acute small bowel obstruction: review of 1,061 cases. Surg Endosc 21:1945-1949, 2007.
8. Kirshtein B, Roy-Shapira A, Lantsberg L, Avinoach E, Mizrahi S. Laparoscopic management of acute small bowel obstruction. Surg Endosc 19:464-467, 2005.
9. Miller G, Boman J, Shrier I, Gordon PH. Etiology of small bowel obstruction. Am J Surg 180:33-36, 2000.
10. Bizer LS, Liebling RW, Delany HM, Gliedman ML. Small bowel obstruction: the role of nonoperative treatment in simple intestinal obstruction and predictive criteria for strangulation obstruction. Surgery 89:407-413, 1981.
11. Harris EA, Kelly AW, Pockaj BA, Heppell J, Hentz JG, Kelly KA. Reoperation on the abdomen encased in adhesions. Am J Surg 184:499-504, 2000.
12. Kahi CJ, Rex DK. Bowel obstruction and pseudo- obstruction. Gastroenterol Clin North Am 32:1229-1247, 2003.
13. Gutt CN, Oniu T, Schemmer P, Mehrabi A, Buchler MW. Fewer adhesions induced by laparoscopic surgery? Surg Endosc 18:898-906, 2004.
14. Bastug DF, Trammell SW, Boland JP, Mantz EP, Tiley EH III. Laparoscopic adhesiolysis for small bowel obstruction. Surg Laparosc Endosc 1:259-262, 1991.
15. Chopra R, McVay C, Phillips E, Khalili TM.Laparoscopic lysis of adhesions. Am Surg 69:966-968, 2003.
16. Duepree HJ, Senagore AJ, Delaney CP, Fazio VW. Does means of access affect the incidence of small bowel obstruction and ventral hernia after bowel resection? Laparoscopy versus laparotomy. J Am Coll Surg 197:177-181, 2003.
17. Sato Y, Ido K, Kumagai M, Isoda N, Hozumi M, Nagamine N, Ono K, Shibusawa H, Togashi K, Sugano K. Laparoscopic adhesiolysis for recurrent small bowel obstruction: long-term follow-up. Gastrointest Endosc 54:476-479, 2001.
18. Szomstein S, Menzo E, Simpfendorfer C, Zundel N, Rosenthal R. Laparoscopic lysis of adhesions. World J Surg 30:535-540, 2006.
19. Beck DE, Opelka FG, Bailey HR, Rauh SM, Pashos CL. Incidence of small bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum 42:241-248, 1999.
20. Akman PC. A study of five hundred incisional hernias. J Int Coll Surg 37:125-142, 1962.
21. Luijendijk RW, Hop WCJ, van den Tol MP, de Lange DCD, Braaksma MMJ, IJzermans JNM, Boelhouwer RU, de Vries BC, Salu MKM, Wereldsma JCJ, Bruijninckx CMA, Jeekel J (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343:392-398, 2000.
22. Franklin ME Jr, Dorman JP, Pharand D. Laparoscopic surgery in acute small bowel obstruction. Surg Laparosc Endosc 4:289-296, 1994.
23. Ibrahim IM, Wolodiger F, Sussman B, Kahn M,Silvestri F, Sabar A. Laparoscopic management of acute small-bowel obstruction. Surg Endosc 10:1012-1015, 1996.
24. Caprini JA, Arcelus JA, Swanson J, Coats R, Hoffman K, Brosnan JJ, Blattner S. The ultrasonic localization of abdominal wall adhesions. Surg Endosc 9:283-285, 1995.
25. Leon EL, Metzger A, Tsiotos GG, Schlinkert RT, Sarr MG. Laparoscopic management of small bowel obstruction: indications and outcome. J Gastrointest Surg 2:132-140, 1998.
26. Suter M, Zermatten P, Halkic N, Martinet O, Bettschart V. Laparoscopic management of mechanical small bowel obstruc- tion: are there predictors of success or failure? Surg Endosc 14:478-483, 2000.
27. Wullstein C, Gross E. Laparoscopic compared with con- ventional treatment of acute adhesive small bowel obstruction. Br J Surg 90:1147-1151, 2003.
28. Boudiaf M, Soyer P, Terem C, Pelage JP, Maissiat E, Rymer R. CT evaluation of SBO. Radiographics 21:613-624, 2001.
29. Frager D, Medwid SW, Baer JW, Mollinelli B, Friedman M. CT of SBO: value in establishing the diagnosis and determining the degree and cause. AJR Am J Roentgenol 162:37-41, 1994.
30. Hodel J, Zins M, Desmottes L, Boulay-Coletta I, Jullès MC, Nakache JP, Rodallec M. Location of the transition zone in CT of small-bowel obstruction: added value of multiplanar reformations. Abdom Imaging 34:35-41, 2009.
